Utilizing 3D printing for prosthetic limbs in developing nations and conflict zones
Craft Research Volume 11 Number 1
© 2020 Intellect Ltd Article. English language.
doi: https://doi.org/10.1386/crre_00013_1
Received 23 August 2019; Accepted 14 December 2019
This article was adapted from my original master's thesis for inclusion in the Craft Research peer-reviewed journal.
Abstract
Traditional methods of prosthetics fabrication are slow, messy, inaccessible and prohibitively expensive, particularly in developing nations and conflict areas. The development of 3D printing technology allows for prosthetics to be made cost-effectively with an added degree of customization and personalization not previously utilized. 3D printing is quickly expanding in the field of prosthetics, but has rarely been implemented in developing nations or countries in armed conflict, despite these areas having the largest number of amputees and the greatest shortage of prosthetics. Resource-poor areas can use 3D printing as a means of providing prosthetic care for local amputees, as this technology is uniquely suited to help amputees acquire high-quality, affordable, comfortable prosthetics. The use of 3D printing can fulfil the critically unmet need for culturally appropriate prosthetic technology and alleviate many of the psychosocial effects suffered by amputees worldwide, but only if such programmes are implemented properly. This synthesized literature review provides information on the process of, usage for and benefits of utilizing 3D printing for prosthetic limbs.
Introduction
The aim of this review is to analyse the use of 3D printing as a means of prosthetics fabrication compared to traditional fabrication methods and how a better design process can produce better prosthetic limbs for amputees. Standards for prosthetic fabrication and distribution in developing nations and conflict areas are explored, as well as how the choice of material and method of fabrication influence the outcome of a prosthetic. 3D printing programmes currently utilized by governmental bodies, non-profit organizations and health clinics around the world (Belliveau 2016), e.g. the International Committee of the Red Cross (ICRC) and Médecins sans Frontières (MSF) (Steen and Heim 2000), are analysed to establish a series of factors that prosthetists should consider when designing limbs, such as the patient’s culture, local geography or terrain and psychological concerns. Using these factors combined with 3D printing, prosthetists can craft a functional prosthetic for a patient’s specific needs that is more comfortable and cost-efficient. The review consists of a background review to provide context and demonstrate the scale of the problem, before introducing, reviewing and comparing prosthesis-fabrication methods.
Methods
A thorough literature review was conducted, searching online databases PubMed and Medline, using search terms such as ‘prosthetics manufacturing’, ‘prosthetics design’, ‘additive manufacturing in medicine’, ‘3D printing in conflict zones’, ‘solutions for traumatic amputations in developing nations’ or ‘best practices for 3D printed prosthetic design’ for relevant full-text articles written in English. Since the first 3D printer was created in 1983 (Hull 1986), but 3D printing prosthetics was not normalized until the late 2000s (Eshraghi et al. 2013), articles were restricted to those published after 1995 to ensure that the content would still be relevant. It should be noted, however, that some amputation evaluation methods were introduced before 1995 and are still considered the standard; therefore, these are included in this review. Overall, 132 articles were reviewed and 84 were used in this final review. The remaining 48 articles were excluded due to their use of outdated technology or research, or their attention to details beyond the scope of this review.
Background
The use of prosthetic technology can be traced back to ancient Egypt, where archaeologists found a 3000-year-old carved wooden toe attached to a leather strap. Since then, through the increasing scale of wars and global conflict, the need for decent prosthetic devices has significantly increased (Anderson and Perry 2014), leaving the medical industry in urgent need for new methods of prosthesis manufacture.
Amputation global disease burden
The burden of amputation disproportionately affects people of low-income countries and is aggravated by disparities in medical supplies, trained health workers and overall care. There are over 35 million people living with limb loss worldwide (WHO 2017), 80 per cent of them in developing countries and conflict areas (Harkins et al. 2012). Less than 10 per cent of amputees in low-income countries requiring a prosthetic have access to them (Borg et al. 2011).
Trauma-related amputations are most common in developing countries and, as such, are the primary focus of this article. Trauma can include everything from stepping on a landmine to industrial accidents. India, with its overcrowded urban areas and precarious transportation, sees up to 14,000 amputations a year due to train accidents (Staats 1996). The 2010 earthquake in Haiti is thought to have caused more amputations than any other single event in history, requiring between 6000 and 8000 (Kelly 2010). For those living in armed conflict, such as the people of Yemen, gunshot wounds, mortars, artillery shells and landmines are the likely causes of amputation (Al-Ganadi 2015). An estimated 80,000–200,000 amputations were performed in the first five years of the Syrian crisis (Sebai et al. 2016). By the end of Sri Lanka’s 26-year war, there were approximately 160,000 amputees in the country (Dathan 2018). Landmines still active in many regions continue to cause traumatic amputations for local citizens, mostly children, in post-war societies (Prasad and Prasad 2009).
Studies have shown that patients in developing countries, particularly conflict zones and refugee populations, often seek out or receive medical attention when it is too late to salvage the limb, making them more susceptible to amputations (Chalya et al. 2012). Surgeons in a reconstructive surgery hospital treating Syrian, Libyan and Palestinian refugees in Jordan reported that over 50 per cent of their patients arrive with chronic infections (60 per cent of which are multidrug resistant), increasing the likelihood of amputation (Médecins Sans Frontières 2017). Therefore there is a heightened need for prosthetic devices in such areas.
Furthermore, in areas of conflict where infrastructure is often crumbling, amputees may have to navigate makeshift roads with potholes or climb rugged mountainous terrain. They may have to take care for themselves and their families, find economic stability and manage the psychosocial impacts of being an amputee, generally without access to medical support facilities of any kind. Having a functional prosthetic tailored to a patient’s specific needs can enable them to manage these challenges (Marks and Michael 2001).
Types of prosthetics
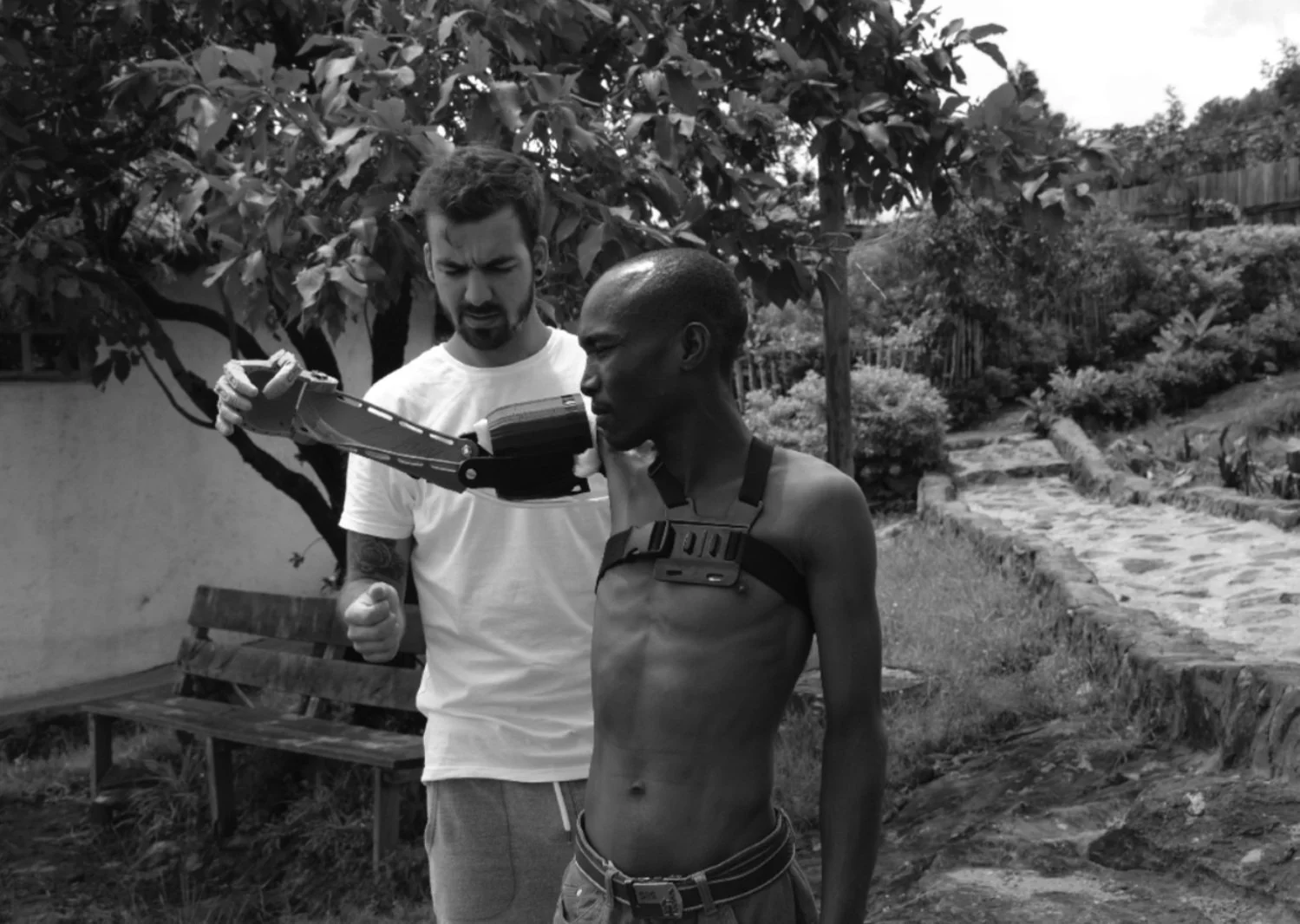
Prosthetic limbs range from simple cosmetic devices (limbs with rudimentary functionality that give the appearance of a normal limb) to high-tech machinery (Clark 2014). Upper limb prosthetics can utilize lower-tech designs, like a high-tension string mechanism, seen in Figure 1, or high-tech electronic components, such as microprocessors, to allow for a certain degree of mental control over the limb (Jiang 2017). This phenomenon, called myoelectricity, allows amputees to use the remaining muscles in the residual limb to signal sensors in the socket as to their intended action, allowing the hand or arm to ‘move’ with relative fluidity (Service 2018). Such sensors are less likely to work in lower limb prosthetics as the body’s weight pressing down on the socket makes the myoelectric sensors less able to pick up on the electrical signals under the skin.
Legs also present different sets of problems as movements of the knees, ankles and feet are less conscious and more autonomous than movements of the hands, wrists and fingers (Mooney et al. 2014). They also have to provide a certain amount of support for the amputee. Lower limb prosthetics make use of passive systems, largely based on mechanical joints. In particularly advanced prosthetics, mechanical joints, often called active joints, can automatically adjust stiffness while walking, allowing an artificial knee to bend and straighten with each step (Nathan 2018). Amputees with older prosthetics not fitted with mechanical joints recount having to hold their prosthetic knee together while in the standing phase of a walking gait to keep their prosthetic from collapsing, but then manually bending the joint mid-stride to keep it from locking up (Reiber et al. 2010). Active joints fix this problem through the use of actuators (components responsible for movement and
control) in the form of either electromechanical units (mechanical devices using electrical energy), pneumatic units (gas- or air-powered devices), hydraulic units (powered by the movement of a liquid) or variable impedance actuators (an elastic element within the device that can store energy and reuse it during various phases of gait).
All of these active joints use mechanical properties to simulate the act of human locomotion (Mooney et al. 2014). These actuators not only provide a more realistic gait, but in advanced cases, can also automatically adjust to changes in posture on uneven surfaces, making them more stable in irregular conditions, such as an amputee farmer’s terraced rice field (Howard et al. 2017). In resource-poor areas, active joints are often considered fantastical as few can afford or construct them.
Challenges of traditionally fabricated prosthetics
Conventional prosthetics are made using plaster to create a mould of the residual limb, colloquially called the stump. The mould is then used to create the socket, and the remaining prosthetic is manufactured (often mass-produced) as an average limb (Marks and Michael 2001). Calcined gypsum, known as plaster of Paris, must be mixed with water and generously applied to plaster bandages, which are then wrapped around the residual limb (Asbelle and Porter 1972). Crystallization occurs within a few minutes of mixing and quickly enters the setting stage, at which point there should be no further manipulation of the plaster to obtain an accurate mould. Prosthetists move quickly and plaster often drips on the floor or is flung onto a wall during the haste. Once the mould sets, it takes roughly twelve–eighteen hours to fully dry in an oven, or up to three full days if no oven is available (Asbelle and Porter 1972). Following drying, the socket can begin to be produced, taking anywhere from a day to two weeks depending on the resources used and availability of staff. After the socket is created, it is paired with an appropriately sized artificial limb that is typically mass-produced and imported from factories (namely in India, China and Korea) (Golovin et al. 2018). The whole process might leave a patient waiting in a hospital bed for several days or weeks (Asbelle and Porter 1972).
In addition, traditional prosthetics are often one-size-fits all, or are so generic that some patients require surgery to fit the patient to the prosthetic (Thurston 2007). Even with a custom plaster mould for the socket, traditional prosthetics are rarely fitted to the patient. Over 95 per cent of amputees using a prosthetic report socket discomfort as a direct result of inaccurate size or shape (Herbert et al. 2005). Although a great deal of design effort can be put into a traditional prosthetic to create a life-like limb – much in the same way a sculptor will spend hours, days or weeks moulding their creation – there can still be little effect of those designs felt by the patient.
Given the large quantity of prosthetic devices needed, the high costs and the difficulties in producing and fitting traditional ones, the proposition is that 3D-printed prosthetics can offer a possible solution through better fit, added strength to hold up under stress, such as use in rough terrain, and are less expensive, making them more affordable to those who need them most. For example, with the use of 3D printing, each component of an active joint can be printed individually and assembled to create a functional prosthetic limb with more natural functionality (Phillips et al. 2017) and that is relatively less expensive.
3D printing of prosthetic devices
The process of 3D printing
In 1983, the first 3D printer was created by Charles Hull and utilized a type of 3D printing known as stereolithography (Hull 1986). 3D printing of finished artefacts, also called rapid manufacturing for its relatively fast production time, creates 3D objects from a digital file, known as a standard tessellation language (STL) file (Bhatia and Sharma 2014). The process has been used in a number of industries, but has recently been improved for use in the medical field, providing more opportunities for patient-specific care.
The process can also be called additive manufacturing as it involves adding layers upon layers of material. Each layer, ranging from 1–7 mm thick, forms a thin, horizontal cross-section, which is laid on top of the previous layer to create the vertical build (Ballard et al. 2017) and then bonded, usually through a heating element, such as a laser, electron beam or plastic-melting nozzle (Gross et al. 2014).
Although stereolithography is the most common kind of 3D printer, there are currently over half a dozen types of 3D printing, including electron beam melting (EBM) and selective laser sintering (SLS), processes that are the focus of this article. Through EBM, a powerful electron beam, encased in a vacuum, melts metallic powders. As this electron beam hits a thin layer of material, it can selectively join or weld these particles together, producing an accurate shape. After each print cycle, a new layer of powdered metal is raked over the existing material, the build platform is lowered incrementally and the next layer is created.
Although EBM can only use metal materials, SLS can use metal, nylon, ceramic, glass or plastic. This process uses high-power CO2 lasers to fuse powdered particles together. The laser sinters, or welds, the powders together, lowering the build platform with each successive layer. As the lasers are extremely precise and only sinter the particles they need for the object build, the remaining particles in the build platform act as supports for the product, ensuring a more durable build.
These existing methods of 3D printing, although still more effective and realistic than traditional fabrication, can omit some of the more detailed microstructure of anatomy (Hosny et al. 2018). New studies are constantly looking at adapting the 3D printing technique and design to further support medical needs, taking every detail of a piece of anatomy, such as an organ or limb, and essentially duplicating it, using a broad range of printing materials at the same time (Skylar-Scott et al. 2019). However, such multi-material technology is not yet viable and SLS and EBM are currently more adequate and produce better prosthetic limbs for amputees in developing nations and conflict zones
than traditional fabrication.
The process of creating 3D printed prosthetics
3D printing is an approach that can accurately reproduce the internal and external structures of the residual limb, customize it for each individual patient and produce an entire prosthetic (Bhatia and Sharma 2014). Prosthetics can be made using any 3D printing method; however, SLS is often considered the best method to produce prosthetic sockets and high-quality, lower cost variable-impedance mechanical joints largely because of its precision in creating the final product and its use of durable materials. SLS allows for customized sockets to be printed with different materials, such as fibre-reinforced plastic for ultimate stiffness, rubber-like material for more flexibility or impact-resistant plastic, which will reduce pressure on the residual limb (Bhatia and Sharma 2014). On the other hand, EBM can provide the most durable metal prosthetic limbs to attach to a socket. Because EBM can only use metal as a material, which is uncomfortable for use as a socket, resource-poor areas that may not have the capability to use both SLS and EBM printing techniques typically rely solely on SLS technology. As mentioned earlier, new printing methods are currently under development that could feasibly make 3D-printed prosthetic limbs still more reliable and realistic, using up to seven different types of material; however, the research and cost behind them may not be attainable for resource-poor areas for some time (Skylar-Scott et al. 2019).
Before any prosthetic parts can be printed, they have to be scanned and designed. A portable 3D scanner – roughly the size of a tea kettle – can scan the precise dimensions and shape of any 3D object and send them wirelessly to a fabrication centre (Breitegger and Kollatsch 2018). The scan creates a 3D image that is imported into a 3D modelling program as a Computer-Aided Design (CAD) file (Lee et al. 2017). As mentioned earlier, 3D printers work off of STL files, but CAD software uses CAD files to design and manipulate the prosthetic image and design. Once the design is complete and ready to be printed, the CAD software can export the design as an STL file.
In the case of prosthetics, a scan is taken of the residual limb and of the contralateral (on the opposite side of the body) limb (Bhatia and Sharma 2014). The scan of the stump will create a custom socket that allows for a better fit on the amputated limb than traditionally possible, making it more comfortable and increasing adherence to wearing the prosthetic. If a prosthetic fits and is comfortable, patients are more likely to use them regularly (Desmond et al. 2008). The need for a precise fit is much like finding a proper pair of shoes: too big and it is difficult to walk, but too small and it becomes painful to wear. Once the design is finished, the software slices the 3D image into hundreds of horizontal layers. The sliced image is transmitted to the 3D printer, which begins the fabrication process outlined above.
Advantages of 3D printed limbs over traditional prosthetics
The new methods of 3D printing have a number of advantages, including cost, accessibility and customization, which are discussed in the following.
Cost
Traditional prosthetics manufacturing techniques are subtractive, meaning that a large chunk of aluminium, titanium, acrylic, plastic or other material is slowly stripped away until the desired shape is achieved, leaving up to 90 per cent of the original raw materials on the production floor. This can be a tremendous waste of expensive materials for prosthetics clinics operating in low-income and impoverished areas.
A traditionally produced average limb currently available to rural amputees in developing nations is $700 for the limb alone. This does not account for the cost of transportation to a hospital, rehabilitation services, limb maintenance or extra hospital fees associated with fitting the prosthetic (Agence France-Presse 2018). In these same regions, a working person must live on less than $2 a day, making a traditional prosthetic an unreachable dream. Similarly, the most basic, traditionally made cosmetic arm can cost a few hundred dollars, while a 3D printer can make a cosmetic hand for $20 worth of raw materials (Zuniga et al. 2015). A myoelectric hand can cost several thousand dollars when made using traditional processes, while a comparable hand can be 3D printed and fitted with small sensors for roughly $300 (Gretsch et al. 2016). A full cost breakdown is beyond the scope of this article, but a comparison of prices and an overview of fabrication laboratory set-up costs is presented in Table 1.
Portability and accessibility in difficult terrain
Traditional prosthetic manufacturing, not to mention the MRI and CT scanning, is done in urban hospitals (Baronio et al. 2017), making it difficult for countries with largely rural populations to bring prosthetic services to those who need them most. The long distance to a hospital or clinic can be arduous to traverse for amputee patients. They must then remain in the hospital for an average of five days minimum, causing child amputees to miss school or adult amputees to miss work for long periods of time, further impacting their socio-economic status (Bustreo et al. 2005).
There are also obstacles for health workers to reach rural patients (Harkins et al. 2012). The plaster alone, which comes in 20kg bags, would take an extraordinary amount of manpower to continually bring to rural villages. In some African nations, up to 90 per cent of the total population is located in rural areas, meaning that the traditional method of fabricating prosthetics is not practical for nine out of ten patients (Phillips et al. 2016).
Portable scanners used for 3D printing, however, can be packed up easily by trained health workers and taken to rural villages, remote atolls in island nations and even behind enemy lines in war zones to obtain scans of an amputee (Starr 2017). The information is then transmitted wirelessly or via satellite to a centrally located fab lab, which can begin printing the limb, altogether increasing access. High-efficiency 3D printers are now being built with solar panels, eliminating the need for expensive generators (Gwamuri et al. 2016).
Customization capabilities of 3D printing
One of the most remarkable things about 3D-printed prostheses is the capability for mass personalization. Traditional prostheses already require a certain amount of customization to account for the location of the amputation and the size of the patient – a child with a transfemoral* amputation will need a full leg prosthetic in a smaller size than a grown man with a transtibial** amputation. Some customizability is also given through the functionality of a traditional prosthetic depending on if sensors are used for a myoelectric hand or if a transradial*** amputee requires only a nonfunctional cosmetic hand.
With 3D printing, however, the customizability of a prosthesis can be truly endless, starting with the fit of the prosthesis. For example, a woman with a transtibial amputation can walk six miles to fetch water because her socket has varying degrees of stiffness, providing strength on the outside, with a higher degree of comfort on the inside sleeve (Herbert et al. 2005). The microstructure of a prosthetic can be customized for each patient. Lower limb prostheses can be printed with complex internal geometries that will help a subsistence farmer stay balanced on uneven terrain. Parts for a variable-impedance mechanical joint can be printed to mimic a person’s natural gait, reducing stress on his or her contralateral hip (Mooney et al. 2014). Factory workers with transhumeral**** amputations can receive arms fitting their residual limbs so well that they decrease discomfort and the likelihood of socket sores (Highsmith and Highsmith 2007). Prosthetics made by 3D printing can also be incredibly lightweight, with rotating pieces that can help orient a prosthetic for better functionality, as seen in Figure 3. Traditional lower limb prosthetics that are heavy are not only uncomfortable for the patient, but are shown to eventually be discarded in favour of crutches or wheelchairs, despite those being especially difficult in rainy climates and mountainous or agricultural terrain (Kam et al. 2015).
Customization can further occur in the visual appearance of a 3D-printed prosthetic. Filaments can be tinted to match a person’s skin tone exactly, giving a patient the normalcy they may desire. On the other hand, prosthetic limbs can be printed to look entirely unique and patients may want them to be an extension of their personality. A child being bullied because of his or her condition may want an arm that looks like Elsa from Frozen, Iron Man or The Hulk – evoking pride and confidence. Skin-coloured or ‘cool-looking’ prosthetics help patients avoid stigmatization that they may otherwise face because of their deformity (Rybarczyk et al. 1995). A company in Canada even designs
decorative prosthetic covers, giving amputees the opportunity to use their prosthetic as a fashion statement (Jagannathan 2018).
In summary, advances in technology have made 3D printing a viable option for prosthetic fabrication, compared to traditionally made prosthetics, with results being customizable, more durable and less stigmatizing, and with new methods being less time consuming, less expensive and increasingly accessible, particularly in resource-poor areas.
Manufacture of 3D-printed prosthetic devices: Contextual consideration
Resource materials for 3D printing
Prosthetics have been made using a number of different materials, varying greatly by country. Resource-poor nations often look to wood and resin for their limb material, but in farm-based economies, which have harsher, tropical climates, these limbs barely last 18 months (Strait 2006). Limbs in developing nations have also been crafted from bamboo, PVC piping, cloth rags, old tires or bicycle parts. Even when components are imported from industrialized countries, these parts are simply not made to withstand specific challenges of harsh terrain, rural environments and varied lifestyles (Strait 2006).
3D printers can use a variety of materials and, depending on the type of prosthetic, orthosis or implant needed, different materials or a combination of materials can be used to achieve the desired goal. Prosthetists can select a printable material that will allow the limb to retain its strength, while remaining lightweight, and not be detrimental to the patient’s health irrespective of climate, patient’s condition or location. For example, bone implants can be 3D printed with calcium phosphate using specific internal geometries to produce 65 per cent porosity of the material, the same porosity as the bone that it is replacing (Mehrban et al. 2010).
Prosthetists in Sri Lanka took advantage of the country’s booming rubber exports to source local materials, using the cultivated rubber to support the framework of a prosthetic, creating a stronger, less expensive limb (Gunasekera 2017). Syria has an abundance of fibreglass, often used to fix boats for fishermen. As a result, some organizations inside the war-torn country and its neighbours have begun using the fibreglass as a filament for 3D printers, producing sturdy prosthetics for Syrian amputees. Programmes that utilize local resources have lower costs and a faster turnaround time than programmes reliant on imported material.
Plastic salvaged from the ocean can even be separated, shredded, sanitized and melted down into filament reels ready for use in a 3D printer (Srubar and Zhang 2016). This innovative solution addresses two major issues and can conceivably be implemented in coastal communities or island nations with few other local resources. Plastic filaments may have durability and longevity issues, and thus may not be the best resource for long-term prosthetic usage, but can be reasonable for use in limbs for young children who typically need a new prosthetic every six months (Strait 2006). Researchers working on 3D printed prosthetics have also made progress in stress-testing plastics used in sockets, like those in Figure 4, to determine ideal thickness and filling to support a patient’s weight (Braga 2014).
Setting up fabrication laboratories
For politically unstable regions or those currently in armed conflict, the most difficult part of a 3D printing prosthesis programme will be getting a 3D printer into the country. The ease of use and ability to print almost anything makes 3D printing a technique utilized by soldiers, insurgents and armed personnel to create guns, bombs and other weapons of war. Governments are becoming increasingly hesitant to allow such technology into conflict regions. Every country or region will have different rules and regulations on the use of 3D printing and should be thoroughly researched before plans for a fab lab can be established. Some developed countries, like the United States and Australia, are beginning to review 3D-printing materials and methods. The need for Food and Drug Administration (FDA) approval on materials, printers and process of fabrication has left the United States behind many countries who are actively using 3D printing in biomedical research, surgical settings and prosthetic/orthotic fabrication (Tetsworth and Mettyas 2016). The best international guidelines for prosthetics creation, distribution and quality assurance come from the World Health Organization (WHO 2017) and the International Committee of the Red Cross (ICRC) (2007) and should be utilized in conjunction with the local government approval processes. A number of international resources, such as the National Institute of Health (NIH)’s 3D Print Exchange (2018), also provide tips, tools and models for programmes looking to use 3D printing in the medical field.
Workforce needed
The WHO estimates that there is a shortage of 40,000 trained prosthetists in low-income countries (WHO 2005). There are an estimated two million amputees in the Philippines requiring prosthetics, but only nine fully trained experts in the country (Birrell 2017). Many prosthetics-fitting programmes have simply brought prosthetists to a region for a short amount of time to fit amputees in that area. While this works for a week or a month at a time, the shortage of trained personnel still exists and will be further exacerbated when the prosthetists leave and no one is left to maintain prosthetics or refit them as an amputee may grow dissatisfied with them. Most developing nations simply do not have the workforce of skilled professionals needed to provide prosthetic limbs to the majority of patients in their region. 3D printers have the ability to do the actual fabrication, but a gap in computer-aided design skill persists. Specialized CAD tools, such as Autodesk Meshmixer, can streamline this process, and inclusive designers like Dr. Matt Ratto and his colleagues have further added features to simplify the prosthesis design process for prosthetists working with little to no formal design training (Schmidt 2016).
Rehabilitation services are also key to ensure that patients know how to use their prostheses and can recover properly from their trauma. However, a lack of personnel has made these services scant in developing nations (Sinha 2013). Less than 5 per cent of patients in low-income countries who need rehabilitation services have access to them (Sam et al. 2004).
The best prosthetics programmes are those that train local people for prosthetics services, as this starts a cycle of prosthetic education. The WHO provides Guidelines for Training Personnel in Developing Countries for Prosthetics and Orthotics Services (2005), a manual for the education of local prosthetists, which should be utilized during the training process.
Best practices: Design considerations
Initiatives utilizing 3D printing for prosthetics manufacturing should apply a Quality by Design (QbD) approach, outlined by Martinez-Marquez et al. (2018). Particularly because government oversight and protocols can vary, QbD ensures that products are designed and fabricated without error from beginning to end. It employs eight main steps, including (1) target product profile, (2) critical quality attributes, (3) process flow diagram, (4) process parameters/material attributes, (5) risk assessment, (6) design space, (7) control strategy and (8) product life cycle management/continuous improvement, to allow for an in-depth understanding of the needs of the community and the product being created.
Evaluating patients
A proper evaluation is the first and perhaps most important step in determining the best design for each prosthetic. Health workers can be trained to evaluate a patient’s quality of life using evaluation/measurement instruments such as the 36-Item Short Form Health Survey (SF-36) (Ware and Sherbourne 1992), the Sickness Impact Profile (SIP) (Bergner et al. 1981), the Prosthesis Evaluation Questionnaire (PEQ) (Legro et al. 1998), the Barthel Index (Mahoney and Barthel 1965), the Locomotor Capabilities Index (LCI) (Franchignoni et al. 2002), the Functional Independence Measure (Granger et al. 1986) or the amputee mobility predictor with prosthesis (AMPPro) (Gailey et al. 2002).
Workers should also identify each patient’s greatest perceived loss – the one thing an amputee can no longer do that is the most painful (either physically or emotionally). In some cases, this can be walking or running, as it was with a young girl named Roseline in Uganda, seen in Figure 5, who received a simple, yet functional lower limb prosthetic. Other times, it may be a patient’s ability to brush their hair again, pointing to a need for a simple cosmetic device with gripping capabilities. For one man, his greatest perceived loss was his ability to swim with his children, leading researchers to develop and 3D print an amphibious prosthetic leg, with a cone-like shape and holes in the side to allow water to pass through and create propulsion (Eschen 2017). When workers are trained to properly evaluate patients and their needs, they can better understand what kind of prosthetic the patient is looking for, and therefore design a prosthetic better suited for the patient’s individual needs.
Intentional prosthesis design
When prosthetic limbs are designed with purpose and intent, they can better benefit those who rely on them. Careful and customized design of a prosthetic seems to exist only in the developed world. For example, 1600 US soldiers serving in Afghanistan and Iraq have required amputation (Cid de leon Ovalle 2016). With the help of decent prosthetics, at least 167 of these soldiers have remained on active duty, further illustrating the disparities of prosthetic limb distribution in high- versus low- income countries (Koebler 2012).
The design of a prosthetic will depend on a number of factors previously discussed, but can also change according to a patient’s culture, geographic location or even walking speed for lower limb amputees. Patients who walked at a fast pace pre-amputation may benefit from energy storage and return feet (ESAR), meaning that a carbon structure works like a leaf spring, storing energy when in the standing phase, but releasing it during the push-off phase of walking (Au et al. 2008). A better design for these patients might also include an artificial ankle with a more natural (and therefore higher) range of motion, allowing the patient to walk faster according to their own cultural norms (Windrich et al. 2016).
It has been shown that amputees with prosthetics not containing active joints (rather, they use passive or semi-active joints) use more oxygen than amputees with active joints in their prosthetic. This suggests that tasks such as climbing stairs or slopes – or even standing from a seated position – can cause amputees to become more winded and expend more energy for amputees if their prosthetic is designed without active joints (Windrich et al. 2016). While this may seem like a nuanced situation, it may give a prosthetic designer some clue that an amputee Sherpa in Nepal may benefit from a prosthetic with active joints to help them traverse the hilly terrain, or perhaps an amputee living at a high altitude, with less requirement for oxygen, may prefer these active joints. It should be noted that few, if any, scientific studies have been completed on which prosthetic would be best at which altitude, but designers should still consider patients ‘pain points’ and listen if a patient says a prosthetic is too difficult to work under particular conditions (Grimmer and Seyfarth 2014).
Psychosocial effects of prostheses
Amputees in developing countries are highly stigmatized and often shunned from society. The disability has cultural, psychological and physical repercussions for these patients and those who care for them. Limb loss can cause individuals to lose their livelihood, self-confidence and sense of safety in the world. It can affect their economic status, their ability to (find) work and support their families, their marriage prospects or their ability to use transportation to visit health care facilities. The impact of amputation is severe, and the number of patients requiring prosthetics is vast and continually increasing. As such, exploration into the efficacy, efficiency, affordability and design of prosthetic limbs is of the utmost importance.
Adults who have grown up with a limb deformity have been shown to have severe body image issues and often have low self-confidence, particularly if they were bullied about their deformity as a child (Montesinos-Magraner et al. 2016). These adults often want nothing more than to blend in with the general public. 3D printing is uniquely suited to help these patients as a prosthetic can be printed with the exact shape, size, look and even colour as the limb it is replacing. Starting at a younger age, however, this dynamic can be changed entirely, with the help of the same 3D printer, plus some creative designing. Children wearing colourful or bionic-looking limbs are more likely to be asked how the limb works or where they got it, with positive connotations, as opposed to the negative connotations of being asked what happened to them or why they are not like normal children.
Cultural considerations
Cultural norms, such as sitting cross-legged, walking barefoot on rough terrain, use of squatting toilets or genuflecting to elders or in religious ceremonies, can all change the needs for a prosthetic (Harkins et al. 2012). The culture of a specific location can also affect the psychological state of an amputee and therefore their individual prosthetic needs. In Ghana, the disabled/amputee population is thought to be cursed and is ostracized from society, leading to an amputee’s desire for a realistic-looking limb (Kohler et al. 2009). Prosthetists working in Ghana may therefore opt for filaments that are easier to tint to match a patient’s skin tone, as opposed to something sturdier, but monochromatic. In Latin America, however, large families are often economically dependent on the father, and so a man may require a sturdy limb that will allow him to return to work (Harkins et al. 2012).
When culture is taken into account and respected, the local community can provide invaluable support to any prosthetic programme. Universities and other training programmes in the area can be utilized and leveraged to ensure proper training of all personnel, also creating jobs, providing economic stimulation and increasing the likelihood of government and citizen support. By training locals and working with already established community organizations, a 3D printing prosthetics laboratory can become a sustainable business (McGimpsey and Bradford 2017), decreasing the need for outside funding, much like a prosthetic clinic USAID established in Sri Lanka that now operates as an independent, profitable enterprise without further USAID assistance (Gunasekera 2017).
Safety considerations
Limitations still exist in the durability of any prosthetic limb, whether 3D printed or traditionally manufactured. 3D printing is quite capable of making limbs that equal the strength and rigidity of traditional prosthetics; however, great care needs to be taken that quality materials are chosen, and printing speeds are not rushed. Some 3D-printing prosthetic programmes make claims that a limb can be printed and ready for fitting in under four hours. While technically true, these limbs are usually made by stereolithography, with a less rigid thermoplastic, and will not possess the strength or durability truly needed. Prosthetics with quick print times are known to only last a few weeks and can cause serious injuries when eventually worn out.
Lower limb prosthetics are especially problematic when the strength of the limb begins to wane. A number of injuries have occurred when a prosthetic leg breaks while the patient is standing or walking, making durability a key issue (Miller et al. 2001). Cheap or ineffective material used in prosthetics can be detrimental to an amputee’s health. Particularly with lower limb amputees, socket sores and subsequent infections are a real and constant danger when the skin is exposed to harsh material. As the body’s weight bears down on the metal or plastic in a prosthetic, especially in high heat when sweat irritates the residual limb, sores can and likely will occur (Reiber et al. 2010).
The gait of an amputee using a prosthetic leg is also inherently unbalanced (Mooney, Rouse and Herr 2014). In severe cases, substandard, non-functional lower limb prosthetics can cause an uneven gait that imposes extra pressure on the hip bones opposite to the missing leg, resulting in some patients needing a replacement of the hip contralateral to the prosthetic (Kauffman, Barr and Moran 2007). Using great care and better design and fabrication methods, however, 3D-printed prosthetic limbs can help amputees in hard to reach and resource poor regions where quality prosthetics are most needed.
Conclusion
3D printing is uniquely suitable for prosthetics fabrication in developing nations and conflict zones. The materials and methods used are cost-effective for resource-poor nations, portable for rural areas and durable for difficult terrain. 3D printing gives prosthetists the ability to create culturally sensitive, accessible prosthetic limbs that are tailored to each patient’s particular needs, making it the ideal method of prosthetic creation as opposed to traditional fabrication. Prosthetists with a design mindset, who employ craft methods, can further improve the outcome of customized, 3D-printed prosthetic limbs.
*Otherwise known as an ‘Above the Knee’ amputation, a transfemoral amputation occurs through the femur so that the knee is no longer present.
**Otherwise known as a ‘Below the Knee’ amputation, a transtibial amputation is that of the tibia and fibula bones of the lower leg.
***Otherwise known as a ‘Below the Elbow’ amputation, a transradial amputation is that of the radius and ulna of the lower arm.
****Otherwise known as an ‘Above the Elbow’ amputation, a transhumeral amputation is that of the arm at the humerus so that the elbow is no longer present.
References
Agence France-Presse (2018), ‘Lab providing affordable prosthetics for people who’ve lost limbs fighting Islamic State’, The Journal, 25 February, http://www.thejournal.ie/prosthetics-limbs-3867680-Feb2018/. Accessed 2 August 2019.
Al-Ganadi, A. (2015), ‘Management of vascular injury during current peaceful Yemeni revolution’, Annals of Vascular Surgery, 29:8, pp. 1575–80.
Anderson, J. and Perry, H. R. (2014), ‘Rehabilitation and restoration: Orthopaedics and disabled soldiers in Germany and Britain in the First World War’, Medicine, Conflict and Survival, 30:4, pp. 227–51.
Arcam EBM (2018), ‘EBM electron beam melting: In the forefront of additive manufacturing’, Arcam EBM, http://www.arcam.com/technology/electron-beam-melting/. Accessed 5 August 2019.
Asbelle, C. and Porter, G. (1972), ‘Accelerated drying of plaster casts with a microwave oven’, American Orthotic & Prosthetic Association, 26:4, pp. 24–33.
Au, S., Berniker, M. and Herr, H. (2008), ‘Powered ankle-foot prosthesis to assist level-ground and stair-descent gaits’, Neural Networks, 21:4, pp. 654–66.
Ballard, D., Trace, A., Ali, S., Hodgdon, T., Zygmont, M., DeBenedectis, C., Smith, S., Richardson, M., Patel, M., Decker, S. and Lenchik, L. (2017), ‘Clinical applications of 3D printing: Primer for radiologists’, Academic Radiology, 25:1, pp. 52–65.
Baronio, G., Volonghi, P. and Signoroni, A. (2017), ‘Concept and design of a 3D printed support to assist hand scanning for the realization of customized orthosis’, Applied Bionics and Biomechanics, 2017: 8171520, https://doi.org/10.1155/2017/8171520. Accessed 23 July 2019.
Belliveau, J. (2016), ‘Humanitarian access and technology: Opportunities and applications’, Procedia Engineering, 159, pp. 300–06.
Bergner, A., Bobbitt, B., Carter, S. and Gilson, S. (1981), ‘The sickness impact profile: Development and final revision of a health status measure’, Medical Care, 19:8, pp. 787–805.
Bhatia, S. and Sharma, S. (2014), ‘3D-printed prosthetics roll off the presses’, American Institute of Chemical Engineers, 110:5, pp. 28–33.
Birrell, I. (2017), ‘3D-printed prosthetic limbs: The next revolution in medicine’, The Guardian, 19 February, https://www.theguardian.com/technology/2017/feb/19/3d-printed-prosthetic-limbs-revolu tion-in-medicine. Accessed 19 March 2019.
Borg, J., Jindström, A. and Larsson S. (2011), ‘Assistive technology in developing countries: A review from the perspective of the Convention on the Rights of Persons with Disabilities’, Prosthetics and Orthotics International, 35:1, pp. 20–29.
Braga, M. (2014), ‘Inside the 3-D-Printed Limb Factory’, Fast Company, 5 December, https://www.fastcompany.com/3039329/finally-a-good-use-for-3d-printing-prosthetic-limbs. Accessed 9 January 2020.
Breitegger, B. and Kollatsch, J. (2018), ‘3D printing offers new hope to amputees’, Spiegel, 9 July, https://www.industryleadersmagazine.com/3d-printing-is-helping-amputees-in-togo-madagascar-and-syria/. Accessed 2 November 2019.
Bustreo, F., Genovese, E., Omobono, E., Axelsson, H. and Bannon, I. (2005), Improving Child Health in Post-Conflict Countries Can the World Bank Contribute?, Washington, DC: The World Bank Group.
Centene Corporation (2018), Clinical Policy: Durable Medical Equipment and Orthotics and Prosthetics Guidelines, CP.MP.107, St. Louis: Centene Corporation.
Chalya, P. L., Mabula, J. B., Dass, R. M., Ngayomela, I. H., Chandika, A. B., Mbelenge, N. and Gilyoma, J. M. (2012), ‘Major limb amputations: A tertiary hospital experience in northwestern Tanzania’, Journal of Orthopaedic Surgery and Research, 7:18, https://doi.org/10.1186/1749-799X-7-18.
Cid de leon Ovalle, M. (2016), ‘The future of prosthetic technology is here’, Boss Magazine, 16 January, https://thebossmagazine.com/future-prosthetic-technology/. Accessed 2 November 2019.
Clark, L. (2014), ‘Sudanese volunteers are printing £60 limbs in six hours for local amputees’, Wired, 8 January, https://www.wired.co.uk/article/impossible-not-printing-artificial-limbs. Accessed 2 November 2019.
Dathan, J. (2018), ‘The effects of ERW contamination in Sri Lanka’, Journal of Conventional Weapons Destruction, 22:3, pp. 32–36.
Desmond, D., Gallagher, P., Henderson-Slater, D. and Chatfield, R. (2008), ‘Pain and psychosocial adjustment to lower limb amputation amongst prosthesis users’, Prosthetics and Orthotics International, 32:2, pp. 244–52.
Eschen Prosthetics and Robotics Labs (2018), ‘The fin’, Eschen Prosthetics and Robotics Labs, 9 September, https://www.eschenpo.com/prosthetics-the-fin/. Accessed 19 November 2019.
Eshraghi, A., Osman, N. A. A., Gholizadeh, H., Ali, S. and Shadgan, B. (2013), ‘100 top-cited scientific papers in limb prosthetics’, BioMedical Engineering OnLine, 12:119, http://doi:10.1186/1475-925X-12-119.
Franchignoni, F., Tesio, L. and Orlandini, D. (2002), ‘Mobility scales for lower limb-prosthetic patient: The locomotor capabilities index’, Archives of Physical Medicine and Rehabilitation, 83:4, pp. 582–83.
Gailey, R. S., Roach, K. E., Applegate, E. B., Cho, B., Cunniffe, B., Licht, S., Maguire, M. and Nash, M. S. (2002), ‘The amputee mobility predictor: An instrument to assess determinants of the lower-limb amputee’s ability to ambulate’, Archives Physical Medicine and Rehabilitation, 83:5, pp. 613–27.
Gkartzou, E., Koumoulos, E. P. and Charitidis, C. A. (2017), ‘Production and 3D printing processing of bio-based thermoplastic filament’, Manufacturing Review, 4:1, pp. 1–14.
Golovin, M., Marusin, N. and Golubeva, Y. (2018), ‘Use of 3D printing in the orthopedic prosthetics industry’, Biomedical Engineering, 52:2, pp. 100–05.
Granger, C. V., Hamilton, B. B., Keith, R. A., Zielezny, M. and Sherwin, F. S. (1986), ‘Advances in functional assessment in medical rehabilitation’, Topics in Geriatric Rehabilitation, 1:3, pp. 59–74.
Gretsch, K., Lather, H., Peddada, K., Deeken, C., Wall, L. and Goldfarb, C. (2016), ‘Development of novel 3D-printed robotic prosthetic for transradial amputees’, Prosthetics and Orthotics International, 40:3, pp. 400–03.
Grimmer, M. and Seyfarth, A. (2004), ‘Mimicking human-like leg function in prosthetic limbs’, in P. Artemiadis (ed.), Neuro-Robotics: From Brain Machine Interfaces to Rehabilitation Robotics, Berlin: Springer, pp. 105–55.
Gross, B. C., Erkal, J. L., Lockwood, S. Y., Chen, C. and Spence, D. M. (2014), ‘Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences’, Analytical Chemistry, 86:7, pp. 3240–53.
Gunasekera, P. (2017), ‘A locally manufactured foot and a ray of hope for amputees in Sri Lanka’, USAID Frontlines, September/October, https://www.usaid.gov/news-information/frontlines/september-october-2017/locally-manufactured-foot-and-ray-hope. Accessed 20 February 2020.
Gwamuri, J., Franco, D., Khan, K. Y., Gauchia, L. and Pearce, J. M. (2016), ‘High-efficiency solar-powered 3D printers for sustainable development’, Machines, 4:1, pp. 3–15.
Harkins, C., McGarry, A. and Buis, A. (2012), ‘Provision of prosthetic and orthotic services in low-income countries: A review of the literature’, Prosthetics and Orthotics International, 37:5, pp. 353–61.
Herbert, N., Simpson, D., Spence, W. D. and Ion, W. (2005), ‘A preliminary investigation into the development of 3-D printing of prosthetic sockets’, Journal of Rehabilitation Research and Development, 42:2, pp. 141–46.
Herr, H., Wilkenfeld, A. and Blaya, J. (2002), ‘Patient-adaptive prosthetic and orthotic leg systems’, Proceedings of the 12th Nordic Baltic Conference on Biomedical Engineering and Medical Physics, Reykjavik: MIT Media Lab, pp. 123–28.
Highsmith, J. T. and Highsmith, M. J. (2007), ‘Common skin pathology in LE prosthesis users’, Journal of the American Academy of Physician Assistants, 20:11, pp. 33–36.
Hosny, A., Keating, S. J., Dilley, J. D., Ripley, B., Kelil, T., Pieper, S., Kolb, D., Bader, C., Pobloth, A., Griffin, M., Nezafat, R., Duda, G., Chiocca, E. A., Stone, J. R., Michaelson, J. S., Dean, M. N., Oxman, N. and Weaver, J. C. (2018), ‘From improved diagnostics to presurgical planning: High-
resolution functionally graded multimaterial 3D printing of biomedical tomographic data sets’, 3D Printing and Additive Manufacturing, 5:2, pp. 1–11.
Howard, C., Perry, B., Chow, J., Wallace, C. and Stokic, D. (2017), ‘Increased alertness, better than posture prioritization, explains dual-task performance in prosthesis users and controls under increasing postural and cognitive challenge (Research Article)(Report)’, Experimental Brain Research, 235:11, pp. 3527–39.
Hull, C. W. (inventor) and 3D Systems Inc. (assignee) (1986), Apparatus for Production of Three-Dimensional Objects by Stereolithography, Arcadia: US Patent 4575330.
International Committee of the Red Cross (2007), Prosthetics and Orthotics Manufacturing Guidelines, Geneva: ICRC Publications (Reference 0868), https://www.icrc.org/eng/resources/documents/publication/p0868-1.htm. Accessed 23 May 2019.
Jagannathan, M. (2018), ‘This duo wants to do for prosthetics what fashion designers did for eyeglasses’, Market Watch, 6 July, https://www.marketwatch.com/story/this-duo-wants-to-do-for-prosthetics-what-fashion-designers-did-for-eyeglasses-2018-07-06-12883815. Accessed 19 November 2019.
Jiang, P. (2017), ‘Emerging markets are the next frontier of 3D printing’, Entrepreneur, 23 December, https://www.entrepreneur.com/article/305444. Accessed 19 November 2019.
Kam, S., Kent, M., Khodaverdian, A., Daiter, L., Njelesani, J., Cameron, D. and Andrysek, J. (2015), ‘The influence of environmental and personal factors on participation of lower-limb prosthetic users in low-income countries: Prosthetists’ perspectives’, Disability and Rehabilitation: Assistive Technology, 10:3, pp. 245–51.
Kauffman, T. L., Barr, J. O. and Moran, M. (2007), Geriatric Rehabilitation Manual, 2nd ed., Philadelphia: Churchill Livingstone.
Kelly, J. D. (2010), ‘Haitian amputees – lessons learned from Sierra Leone’, New England Journal of Medicine, 362:11, p. e42.
Khasnabis, C. (2015), Standards for Prosthetics and Orthotics Service Provision: 2015–2017 Work Plan (Version 4 September 2015), Geneva: Department of Essential Medicines and Health Products & Management of Noncommunicable Diseases, Disability, Violence and Injury
Prevention.
Koebler, J. (2012), ‘New prosthetics keep amputee soldiers on active duty’, U.S. News & World Report, 25 May, https://www.usnews.com/news/articles/2012/05/25/new-prosthetics-keep-amputee-soldiers-on-active-duty. Accessed 28 July 2019.
Kohler, F., Cieza, A., Stucki, G., Geertzen, J., Burger, H., Dillon, M., Schiappacasse, C., Esquenazi, A., Kistenberg, R. S. and Kostanjsek, N. (2009), ‘Developing core sets for persons following amputation based on the International Classification of Functioning, Disability and Health as a way to specify functioning’, Prosthetics and Orthotics International, 33:2, pp. 117–29.
Lee, K., Bin, H., Kim, K., Ahn, S., Kim, B. and Bok, S. (2017), ‘Hand functions of myoelectric and 3D-printed pressure-sensored prosthetics: A comparative study’, Annals of Rehabilitation Medicine, 41:5, pp. 875–80.
Legro, M. W., Reiber, G. D., Smith, D. G., Del Aguila, M., Larsen, J. and Boone, D. (1998), ‘Prosthesis evaluation questionnaire for persons with lower limb amputations: Assessing prosthesis-related quality of life’, Archives of Physical Medicine and Rehabilitation, 79:8, pp. 931–38.
Lindsey-Curtet, C., Holst-Roness, F. T. and Anderson, L. (2004), Addressing the Needs of Women Affected by Armed Conflict: An ICRC Guidance Document, Geneva: International Committee of the Red Cross, Women and War.
Lu, M., Li, Y., Luo, Y., Zhang, W., Zhou, Y. and Tu, C. (2018), ‘Uncemented three-dimensional-printed prosthetic reconstruction for massive bone defects of the proximal tibia’, World Journal of Surgical Oncology, 16:47, pp. 1–9.
Mahoney, F. I. and Barthel, D. (1965), ‘Functional evaluation: The Barthel Index’, Maryland State Medical Journal, 14, pp. 56–61.
Marks, L. and Michael, J. (2001), ‘Artificial limbs. (clinical review) (science, medicine, and the future)’, British Medical Journal, 323:7315, pp. 732–35.
Martinez-Marquez, D., Mirnajafizadeh, A., Carty, C. P. and Stewart, R. A. (2018), ‘Application of quality by design for 3D printed bone prostheses and scaffolds’, PLoS ONE, 13:4(e0195291), pp. 1–47.
McGimpsey, G. and Bradford, T. C. (2017), Limb Prosthetics Services and Devices; Critical Unmet Need: Market Analysis, Worcester: Bioengineering Institute Center for Neuroprosthetics at Worcester Polytechnic Institute.
Médecins Sans Frontières (2017), Reconstructive Surgery Hospital Amman, Jordan, Amman: MSF.
Mehrban, N., Paxton, J. Z., Bowen, J., Bolarinwa, A., Vorndran, E., Gbureck, U. and Grover, L. M. (2010), ‘Comparing physicochemical properties of printed and hand cast biocements designed for ligament replacement’, Advanced Applied Ceramics, 110:3, pp. 162–67.
Miller, W. C., Speechley, M. and Deathe, B. (2001), ‘The prevalence and risk factors of falling and fear of falling among lower extremity amputees’, Archives of Physical Medicine and Rehabilitation, 82:8, pp. 1031–37.
Montesinos-Magraner, L. I., Issa-Benítez, D., Pagès-Bolíbar, E., Meléndez-Plumed, M., González-Viejo, M. A. and Castellano-Tejedor, C. (2016), ‘Physical and psychosocial functions of adults with lower limb congenital deficiencies and amputations in childhood’, Rehabilitation Research
and Practice, 26:14, pp. 944–53.
Mooney, L. M., Rouse, E. J. and Herr, H. M. (2014), ‘Autonomous exoskeleton reduces metabolic cost of human walking during load carriage’, Journal of NeuroEngineering and Rehabilitation, 11:80, pp. 1–11.
Murphy, D. P. (2014), Fundamentals of Amputation Care and Prosthetics, New York: Demos Medical Publishing, LLC.
Murphy, B., Porcincula, D., Morgan, D., Ruggles, K., Aguayo, C., Mullen, J., Bowman, D. and Laiho, L. (2016), ‘Prosthetic leg kit for deployment in developing countries’, San Luis Obispo: California Polytechnic State University, San Luis Obispo in association with Help One Walk International.
Nathan, S. (2018), ‘Future prosthetic: Towards the bionic human’, The Engineer, 4 January, https://www.theengineer.co.uk/future-prosthetic/. Accessed 19 November 2019.
National Institute of Health (2018), NIH 3D Print Exchange, Bethesda: National Institute of Health, https://3dprint.nih.gov/. Accessed 10 June 2019.
New, J. P., McDowell, D., Burns, E. and Young, R. J. (1998), ‘Problem of amputations in patients with newly diagnosed diabetes mellitus’, Diabetic Medicine, 15:9, pp. 760–4.
Novell, R., Baker, D. M., Goddard, N. J. and Kirk, R. M. (2013), Kirk’s General Surgical Operations, 6th ed., Edinburgh: Churchill Livingstone and Elsevier.
Phillips, B., Ritter, S. and Mehta, K. (2016), ‘Printed prostheses: Not yet ready for developing countries’, Mechanical Engineering, 138:4, pp. 14–15.
Prasad, A. N. and Prasad, P. L. (2009), ‘Children in conflict zones: The human and economic devastation caused by landmines’, Medical Journal Armed Forces India, 65:2, pp. 166–69.
Ranger, B. J. and Mantzavinou, A. (2017), ‘A course in prosthetics for the developing world: Merging education, research and industry to teach biomedical design for social impact’, 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 14 September, Seogwipo.
Reiber, G., McFarland, L., Hubbard, S., Maynard, C., Blough, D., Gambel, J. and Smith, D. (2010), ‘Servicemembers and veterans with major traumatic limb loss from Vietnam War and OIF/OEF conflicts: Survey methods, participants, and summary findings’, Journal of Rehabilitation Research and Development, 47:4, pp. 275–97.
Retfalvi, D. (2017), ‘The perfect fit – how an international team of students designed a solution for third-world amputees’, MedTech Engine, 2 March, https://medtechengine.com/article/amparo-third-world-amputees/. Accessed 5 August 2019.
Rybarczyk, B., Nyenhuis, D. L., Nicholas, J. J., Cash, S. M. and Kaiser, J. (1995), ‘Body image, perceived social stigma, and the prediction of psychosocial adjustment to leg amputation’, Rehabilitation Psychology, 40:2, pp. 95–110.
Sam, M., Childress, D., Hansen, A., Meier, M., Lambla, S., Grahn, E. and Rolock, J. (2004), ‘The “Shape & Roll” prosthetic foot: I. Design and development of appropriate technology for low-income countries’, Medicine, Conflict and Survival, 20:4, pp. 294–306.
Sarvestani, A. S. and Azam, A. T. (2013), ‘Amputation: A ten-year survey’, Trauma Monthly, 18:3, pp. 126–29.
Schmidt, R. (2016), ‘PrintAbility Project’, Toronto: Nia Technologies, http://www.rms80.com/prosthetics. Accessed 3 January 2020.
Sebai, M. E., Bello, R. J., Clarke-Pearson, E., Redett, R. J., Wan, E. L., Manahan, M. A., Sacks, J. M., Cooney, D., Cooney, C. M. and Rosson, G. D. (2016), ‘Severe deficiency of reconstructive surgery for the hidden victims of the Syrian crisis: Challenges and urgent call for solutions for non-fatal injury victims’, Journal of the American College of Surgeons, 223:4, p. e128.
Service, R. F. (2018), ‘New artificial nerves could transform prosthetics’, Science Magazine, 31 May, http://www.sciencemag.org/news/2018/05/new-artificial-nerves-could-transform-prosthetics. Accessed 2 November 2019.
Sinha, R. (2013), ‘Adjustments to amputation and artificial limb, and quality of life in lower limb amputees’, Ph.D. thesis, Groningen: University of Groningen.
Skylar-Scott, M. A., Mueller, J., Visser, C. W. and Lewis, J. A. (2019), ‘Voxelated soft matter via multi-material multinozzle 3D printing’, Nature, 575:7782, pp. 330–35.
Srubar, W. V., Zhang, W. (inventors) and University of Colorado, Boulder (assignee) (2016), Methods of Isolating Melt-Processible Polycarbonate from Plastic Waste, Methods for Preparing Polycarbonate-Containing Hybrid Polymers, and Compositions Comprising Same, Boulder: US Patent US20180105668A1.
Staats, T. B. (1996), ‘The rehabilitation of the amputee in the developing world: A review of the literature’, Prosthetics and Orthotics International, 20:1, pp. 45–50.
Starr, S. (2017), ‘War survivors helped by groundbreaking 3D prosthesis technology’, The Irish Times, 2 August, https://www.irishtimes.com/news/world/europe/war-survivors-helped-by-ground-breaking-3d-prosthesis-technology-1.3173899. Accessed 2 January 2020.
Steen, J. J. and Heim, S. (2000), ‘Evaluation of polypropylene prostheses designed by the International Committee of the Red Cross for transtibial amputees’, Prosthetics and Orthotics International, 24:1, pp. 47–54.
Strait, E. (2006), ‘Prosthetics in developing countries’, Ph.D. thesis, Ames: Iowa State University.
Tetsworth, K. D. and Mettyas, T. (2016), ‘Overview of emerging technology in orthopedic surgery: What is the value in 3D modeling and printing?’, Techniques in Orthopedics, 31:3, pp. 143–52.
Thurston, A. J. (2007), ‘Paré and prosthetics: The early history of artificial limbs’, ANZ Journal of Surgery, 77:12, pp. 1114–19.
Trauner, K. B. (2018), ‘The emerging role of 3D printing in arthroplasty and orthopedics’, The Journal of Arthroplasty, 33:8, pp. 2352–54.
Ventola, C. L. (2014), ‘Medical applications for 3D printing: Current and projected uses’, Pharmacology and Therapeutics, 39:10, pp. 704–11.
Ware, J. E., Jr and Sherbourne, C. D. (1992), ‘The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection’, Medical Care, 30:6, pp. 473–83.
Windrich, M., Grimmer, M., Christ, O., Rinderknecht, S. and Beckerle, P. (2016), ‘Active lower limb prosthetics: A systematic review of design issues and solutions’, Biomedical Engineering Online, 15(Supplement 3):140, http://doi: 10.1186/s12938-016-0284-9.
World Health Organization (2005), Guidelines for Training Personnel in Developing Countries for Prosthetics and Orthotics Services, Geneva: WHO.
World Health Organization (2017), Standards for Prosthetics and Orthotics, Part 1: Standard, Geneva: WHO.
Zuniga, J., Katsavelis, D., Peck, J., Stollberg, J., Petrykowski, M., Carson, A. and Fernandez, C. (2015), ‘Cyborg beast: A low-cost 3d-printed prosthetic hand for children with upper-limb differences’, Boston Medical Center Research Notes, 8:10, http://doi:10.1186/s13104-015-0971-9.
Zuniga, J. M., Dimitrios, K., Peck, J. L., Srivastava, R., Pierce, J., Dudley, D., Salazar, D., Young, K. L. and Knarr, B. A. (2018), ‘Coactivation index of children with congenital upper limb reduction deficiencies before and after using a wrist-driven 3D printed partial hand prosthesis’, Journal of
NeuroEngineering and Rehabilitation, 15:48, http://doi:10.1186/s12984-018-0392-9.
Suggested citation
Rosenberger, Madeline Rae (2020), ‘Utilizing 3D printing for prosthetic limbs in developing nations and conflict zones’, Craft Research, 11:1, pp. 9–38, doi: https://doi.org/10.1386/crre_00013_1
Contributor details
Madeline Rae Rosenberger is a journalist, researcher and anthropologist who holds degrees in journalism and cultural anthropology from Boston University, and a master of public health from The George Washington University. She studied culture and history at Dublin City University and was trained in crisis reporting by the Dart Center for Journalism and Trauma at Columbia University. Based in Los Angeles, California, Madeline focuses on health and culture in developing nations and conflict areas.
Contact: The George Washington University, Washington, DC, 20052, USA.
https://orcid.org/0000-0001-5823-4625
Madeline Rae Rosenberger has asserted their right under the Copyright, Designs and Patents Act, 1988, to be identified as the author of this work in the format that was submitted to Intellect Ltd.






